- Research
- Open access
- Published:
Mechanical force regulates the paracrine functions of ADSCs to assist skin expansion in rats
Stem Cell Research & Therapy volume 15, Article number: 250 (2024)
Abstract
Background
In the repair of massive tissue defects using expanded large skin flaps, the incidence of complications increases with the size of the expanded area. Currently, stem cell therapy has limitations to solve this problem. We hypothesized that conditioned medium of adipose-derived stem cells (ADSC-CM) collected following mechanical pretreatment can assist skin expansion.
Methods
Rat aortic endothelial cells and fibroblasts were cultured with ADSC-CM collected under 0%, 10%, 12%, and 15% stretching force. Ten-milliliter cylindrical soft tissue expanders were subcutaneously implanted into the backs of 36 Sprague-Dawley rats. The 0% and 10% stretch groups were injected with ADSC-CM collected under 0% and 10% stretching force, respectively, while the control group was not injected. After 3, 7, 14, and 30 days of expansion, expanded skin tissue was harvested for staining and qPCR analyses.
Results
Endothelial cells had the best lumen formation and highest migration rate, and fibroblasts secreted the most collagen upon culture with ADSC-CM collected under 10% stretching force. The skin expansion rate was significantly increased in the 10% stretch group. After 7 days of expansion, the number of blood vessels in the expanded area, expression of the angiogenesis-associated proteins vascular endothelial growth factor, basic fibroblast growth factor, and hepatocyte growth factor, and collagen deposition were significantly increased in the 10% stretch group.
Conclusions
The optimal mechanical force upregulates specific paracrine proteins in ADSCs to increase angiogenesis and collagen secretion, and thereby promote skin regeneration and expansion. This study provides a new auxiliary method to expand large skin flaps.
Background
Massive soft tissue defects caused by excision surgery, trauma, burns, and chronic ulcers seriously increase morbidity and mortality, which remains one of the most challenging problems in plastic surgery [1]. Unfortunately, traditional skin flap transplantation has drawbacks including additional damage of the donor site and functional and aesthetic deficiencies.
Tissue expansion can eliminate donor site complications related to long-distance tissue transplantation, and expanded skin tissue has a similar quality as skin in the defective area. Therefore, this technique has been widely used for breast reconstruction, genitourinary system reconstruction, and treatment of giant congenital naevi and other diseases [2]. Nevertheless, as the size of the expanded area increases, the blood supply becomes insufficient and the necrosis rate gradually increases [3]. In addition, some therapeutic factors, such as postoperative radiotherapy for breast cancer, [4] greatly increase the incidence of complications. Mesenchymal stem cells (MSCs) are a promising treatment option due to their unique tissue regenerative capacity. Compared with other types of MSCs, adipose-derived stem cells (ADSCs) have received much attention due to their abundance and simple isolation procedure. However, although stem cells are promising for tissue repair, their use is hindered by problems such as immune rejection and tumorigenicity [5]. In addition, the migration ability, survival rate, and differentiation ability of MSCs decrease after transplantation, which limits their therapeutic potential [6]. Therefore, the development of novel therapies that are safe and effective for expansion of large skin flaps has been intensely pursued.
An increasing body of evidence demonstrates that paracrine function is central to the effects of MSC-based therapy [7]. MSCs can release a variety of functional molecules such as growth factors, inflammatory cytokines, chemokines, and extracellular matrix components. Some studies have shown that conditioned medium of ADSCs (ADSC-CM) has the potential to promote tissue regeneration [8, 9]. However, the composition of the stem cell secretome is affected by numerous factors, including the tissue source, microenvironment, biological behaviors, and physical and chemical stimulation, which hampers its application in regenerative medicine [10]. It may be possible to customize the secretome and develop a cell-free therapy by modulating these factors [11].
Many studies have shown that MSCs can be pretreated with hypoxia, genetic engineering, and physical and chemical stimulation to amplify or inhibit specific biomolecules and thereby achieve the desired therapeutic effect [12, 13]. Among the numerous pretreatment methods, mechanical force has the advantages of simple application, quantitative comparability, and no by-products. MSCs are sensitive to mechanical induction [14]. Mechanical stimulation can induce ADSCs to secrete growth factors, such as vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF), which promote angiogenesis [15, 16]. Previous study found that mechanical forces regulate the migration, differentiation, and paracrine functions of ADSCs to varying degrees [17]. Thus, we hypothesized that application of a specific amount of mechanical force can modulate the paracrine functions of ADSCs to promote skin regeneration. Green nanomaterial is a new field that makes use of sustainable processes and non-toxic ingredients, making it an ideal choice for medical applications [18]. Many studies have shown that nanomaterials can bind to extracellular vesicles obtained by cell paracrine and show great potential in tumor therapy [19]. In addition, the development of nano-scaffolds highlights their great potential in plastic and reconstructive surgery. Therefore, we expect that the combination of mechanically treated ADSC-CM and nanomaterials will make a breakthrough in repairing massive soft tissue defects in the future.
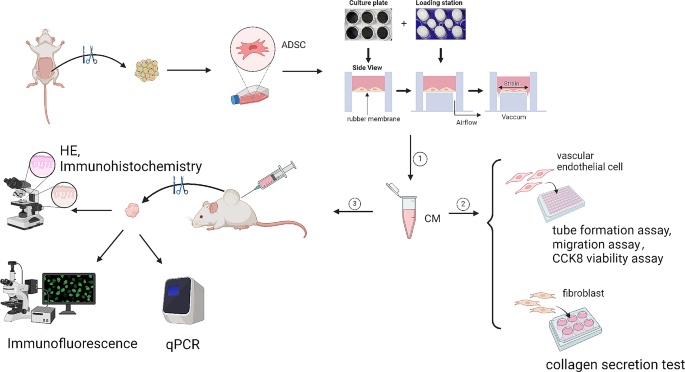
We hypothesized that ADSC-CM collected under specific mechanical forces can promote skin regeneration by facilitating angiogenesis and collagen secretion. To investigate this, we applied different degrees of mechanical force to ADSCs and explored the relationship between the magnitude of mechanical force and the paracrine functions of ADSCs. A rat skin expansion model was used in which ADSC-CM was subcutaneously injected into the expanded area to explore the role of ADSC-CM in skin expansion and the underlying mechanism (Fig. 1).
Materials and methods
Animals
This study was approved by the Nanfang Hospital Animal Ethics Committee and was conducted according to the guidelines of the National Health and Medical Research Council of China. All animals were purchased from Nanfang Hospital Animal Center (Guangzhou, China), without specific pathogens, and were excluded from abnormal or dying animals in the acclimatization period before the experiment. All surgical procedures were performed according to the aseptic principle. The work has been reported in line with the ARRIVE guidelines 2.0.
Cell isolation and culture
ADSCs were isolated as previously described [20]. After shaving, two male Sprague-Dawley (SD) rats (6-weeks-old, n = 2) were sacrificed and subcutaneous fat was harvested. Approximately 4 g of fat was acquired from each rat and stored in a sterile 50 mL centrifuge tube. Subsequently, red blood cells were removed by washing three times with phosphate-buffered saline (PBS, pH 7.4). The isolated fat was cut into small pieces and then digested with 0.2% type Ι collagenase (Solarbio Technology Co., Ltd, Beijing, China) for 60 min at 37 °C with continuous stirring. After digestion, the adipose cell suspension was centrifuged at 800 g for 5 min, and then the cell pellet was resuspended in PBS and filtered through a 100 μm mesh cell strainer. After further centrifugation at 800 g for 5 min, the cell pellet was resuspended in complete growth medium, which comprised Dulbecco’s modified Eagle’s medium: Nutrient Mixture F-12 (DMEM/F12; Gibco, Carlsbad Island, NY, USA) supplemented with 10% fetal bovine serum (FBS, Gibco) and 1% penicillin-streptomycin (Gibco). The cell suspension was then placed in 100 mm culture dishes and incubated at 37 °C with 5% CO2. The medium was changed every 3 days and cells were passaged when they reached 90% confluency. ADSCs were used at passage 2–5.
Rat aortic endothelial cells and dermal fibroblasts (Procell Life Science & Technology Co., Ltd, Wuhan, China) were cultured in Dulbecco’s modified Eagle medium-low glucose (Gibco) containing 10% FBS and 1% penicillin-streptomycin (Gibco). Cells were maintained at 37 °C in a humidified atmosphere of 5% CO2 and 95% air.
Cell stretching and conditioned medium collection
ADSCs were seeded in a silicone rubber membrane coated with type I collagen (Col I) at a density of 1 × 104 cells/cm2 in DMEM/F12 supplemented with 10% FBS. After continuous culture for 24 h, the medium was removed and 2 mL of fresh DMEM/F12 was added to starve cells. After cell starvation, all samples were exposed to static stretch for 6 h using a FX-4000T™ Flexcell® Tension Plus™ unit (Flexcell International Corporation, Burlington, NC, USA), [21] and the conditioned medium was collected. Before the mechanical stretch experiment, the stretching range, frequency, time, and load model were set using the software, and the equipment automatically calculated the required vertical displacement of the rubber membrane, which ensured that cell length was elongated a certain amount in the circumferential direction. We reviewed various cell stretching experiments and found that when the cell elongation rate was between 10% and 15%, the cells maintained a physiological stretching state and avoided apoptosis. Additionally, this range of elongation induced corresponding changes in paracrine, promoting different cellular functions. Based on these findings, four groups (0% stretch, 10% stretch, 12% stretch, and 15% stretch) were included [22,23,24,25].
Cell viability assay
The Cell Counting Kit-8 (CCK-8; Shanghai, Biosharp, China) was used to evaluate the effects of ADSC-CM collected under different mechanical forces on endothelial cell proliferation. Serum-free DMEM or ADSC-CM collected under 0%, 10%, 12%, or 15% stretching force was added into the culture medium, and the cells were incubated for 0, 24, 48 h. After incubation, PBS was used to wash cells for 3 times, and CCK-8 solution (10 µL; 1:10 diluted) was added into the fresh culture medium at 37 °C for 2 h. Finally, the optical absorbance for each sample was measured at 450 nm using an ELISA reader (Thermo Fisher, Massachusetts, USA).
Migration assay
The scratch wound assay was performed to evaluate the effect of ADSC-CM collected under different mechanical forces on endothelial cell migration. Rat aortic endothelial cells were seeded in a 6-well plate at a density of 3 × 105 cells/well. After the cells had reached 90% confluency, a sterile 200 µL pipette tip was used to scratch them vertically. Each scratch was required to be straight and the same in each well. The cells were then washed twice with PBS, and serum-free DMEM or ADSC-CM collected under 0%, 10%, 12%, or 15% stretching force was added. Images were acquired 0, 12, and 24 h after scratching.
Tube formation assay
To evaluate angiogenesis induced by ADSC-CM, rat aortic endothelial cells were seeded into a 96-well plate coated with Matrigel (BD Biosciences, CA, USA) at a density of 3 × 104 cells/well. Matrigel was dissolved overnight at 4°C and placed in each well on ice in advance. ADSC-CM collected under 0%, 10%, 12%, or 15% stretching force or serum-free DMEM was added to each well, and then the cells were cultured for 30 min at 37 °C. The polygonal structures of endothelial cells were observed using an optical microscope 6 h after cell seeding. The tube formation ability was evaluated by calculating the total tube length and total number of nodes.
Collagen secretion assay
To evaluate secretion of collagen induced by ADSC-CM, rat dermal fibroblasts were seeded in a 6-well plate at a density of 5 × 105 cells/well. After the cells had reached 90% confluency, the medium was replaced by serum-free DMEM or ADSC-CM collected under 0%, 10%, 12%, or 15% stretching force, and the culture was continued for 24 h. Collagen secretion by fibroblasts was measured by quantitative real-time PCR.
Skin expansion model
Thirty-six SD rats (6-week-old, male, 250–300 g) were used for in vivo experiments. For sample size calculation, we calculated that the sample size of 3 achieves 90.6% power in 1 weeks and the sample size of 3 achieves 95.2% power with a significance level (α) of 0.05 using a two-sided paired t-test in 30 days according to our pre-experimental results. Three samples per time point were selected in 3, 7, 14, and 30 days. Rats were maintained by routine breeding in the Laboratory Animal Center at Southern Medical University and maintained on a standard chow diet ad libitum in a 12-h light/dark cycle. Three rats were housed per cage. All experimental procedures were approved by the Institutional Animal Care and Use Committee, and were in accordance with their recommendations. Rats were anesthetized with 2% isoflurane, and 10 mL silicon expanders (Guangzhou Wanhe Plastic Material, Guangzhou, China) were subcutaneously implanted on the dorsal side. Thereafter, 15 mL of 0.9% saline was injected through the port of the tissue expander to maintain the same expansion tension in all groups. Rats were allocated randomly to the 10% stretch group (N = 12), 0% stretch group (N = 12), and control group (N = 12) by random number table. In the 0% and 10% stretch groups, ADSC-CM collected under 0% and 10% stretching force, respectively, was subcutaneously injected into the expanded area as soon as the expander was implanted. In the control group, the expander was implanted but no injection was performed. In each group, rats were randomly assigned to four time points, namely, 3, 7, 14, and 30 days (N = 3 per time point). At each time point, full thickness skin specimens were collected from the expanded area to observe the effect of mechanically preconditioned ADSC-CM on skin regeneration. After the samples were collected, the rats were immediately euthanized by inhaling excessive isoflurane and cervical dislocation, and the respiratory rate and heart rate were monitored.
Histological examination
Skin specimens were fixed in 4% paraformaldehyde overnight at low temperature. Subsequently, samples were washed using precooled PBS, dehydrated with different concentrations of ethyl alcohol, embedded in paraffin, and cut into 4 μm thick sections for hematoxylin and eosin (H&E) staining. A microscope (Olympus Corp., Tokyo, Japan) was used to obtain photomicrographs (magnification, ×5). Five H&E-stained regions per group were randomly selected by author in a single-blinded fashion to measure the full thickness of skin using ImageJ software (NIH, Bethesda, MD, USA).
Immunofluorescence and immunohistochemistry
For immunofluorescence assays, after dewaxing, antigen retrieval, dehydration, and blocking, paraffin sections were incubated with an anti-rat CD31 primary antibody (diluted 1:100; Abcam, Cambridge, England) at 4 °C overnight to investigate the level of newly formed vessels. Then, the secondary antibody was applied and sections were incubated for 1 h in the dark. Finally, nuclei were counterstained with DAPI for 15 min. Stained cells were photographed using a fluorescence microscope. To assess angiogenesis, the central and side regions of each sample were compared. To quantitate angiogenesis, the numbers of new capillaries (CD31-positive) in central regions per sample were counted by author in a single-blinded fashion in 100× magnification field.
For immunohistochemistry assays, the paraffin sections were dewaxed, dehydrated, and incubated overnight at 4 °C with anti-Col I (diluted 1:100, Abcam) and anti-type III collagen (Col III; diluted 1:100, Abcam) primary antibodies. After washing, the secondary antibody (diluted 1:100; Thermo Fisher, Massachusetts, USA) was added, and sections were incubated for 1 h at room temperature. Stained cells were developed with diaminobenzidine and counterstained with hematoxylin. To quantitate collagen deposition, the author calculated the average optical density in five fields per sample in a single blind way in 100× magnification field using ImageJ software (NIH, Bethesda, MD, USA).
Quantitative real-time PCR
The total RNA was extracted from the skin samples and fibroblasts with TRIzol® Reagent (Invitrogen, Carlsbad, CA, USA). cDNA was synthesized using EasyScript® First-Strand cDNA Synthesis SuperMix (TransGen Biotech, Beijing, China) according to the manufacturer’s instructions. Quantitative real-time PCR was performed using the PRISM® 7500 Sequence Detection System (ABI, Massachusetts, USA) and FastStart Universal SYBR Green Master Mix (Vazyme Biotech Co., Ltd., Nanjing, China).
Fibroblast samples were tested for type I collagen (Col I), and type III collagen (Col III), and the skin samples were tested for the following genes: VEGF, bFGF, hepatocyte growth factor (HGF) and platelet-derived growth factor (PDGF). Relative expression normalized to expression of β-actin (endogenous loading control) was calculated using the 2−ΔΔCt method. The primer–probe sequences were as follows: β-actin (150 bp), forward 5′-AGGGAAATCGTGCGTGACAT-3′ and reverse 5′-GAACCGCTCATTGCCGATAG-3′; Col I (200 bp), forward 5′-CCTGACGGTGCTATTTAACA-3′ and reverse 5′-GGAAAATGGTGCTCTGAAAC-3′; Col III (170 bp), forward 5′-CCTGAAGATGTCCTTGATGTAC-3′ and reverse 5′- GCCTTGAATTCTCCCTCATT-3′; VEGF (232 bp), forward 5′-AGATTCTGCAAGAGCACC-3′ and reverse 5′-AAGGTCCTCCTGAGCTAT-3′; HGF (160 bp), forward 5′-AAACAAGGTCTGGACTCACATG-3′ and reverse 5′- CCAAGGAACGAGAGGATTCC-3′; bFGF (170 bp), forward 5′-AAGGATCCCAAGCGGCTCTA-3′ and reverse 5′-TCGCACACACTCCCTTGATG-3′; and PDGF (190 bp), forward 5′-ACTCCATCCGCTCCTTTGA-3′ and reverse 5′-GTCTTGCACTCGGCGATTAC-3′.
Statistical analysis
Statistical analyses were performed using SPSS version 25.0 (IBM, Inc., Armonk, NY, USA) with a one-way analysis of variance. Two groups were compared using the least significant difference method or Mann-Whitney U-test. p < 0.05 was considered statistically significant.
Results
ADSC-CM collected under mechanical force promotes migration and angiogenic tube formation of rat aortic endothelial cells
To study the effect of ADSC-CM on angiogenesis and determine the most suitable mechanical pretreatment, we investigated the effects of ADSC-CM collected under different stretching forces on rat aortic endothelial cells. Cells were cultured in ADSC-CM or serum-free DMEM, and the effects of ADSC-CM on proliferation, migration and angiogenic tube formation of these cells were compared. The scratch wound assay demonstrated that migration of these cells was most promoted in the 10% stretch group (8.05 ± 2.20, n = 3, p < 0.0001; 15.55 ± 0.70, n = 3, p < 0.0001) (Fig. 2a b) (Additional file 1). The results of the CCK8 experiment showed that the absorbance changes in each stretching group were not significantly different from those in the control group. (0.953 ± 0.112,n = 3, p > 0.05; 0.968 ± 0.121, n = 3, p > 0.05; 0.989 ± 0.147, n = 3, p > 0.05; 0.853 ± 0.073, n = 3, p > 0.05;0.920 ± 0.074, n = 3, p > 0.05) (Fig. 2c) After cells began to form capillaries, calculation of the length of tubes and number of nodes showed that lumen formation at 6 h was best in the 10% stretch group (1554.00 ± 79.6806, n = 3, p < 0.01; 47504.33 ± 1742.71, n = 3, p < 0.0001) (Fig. 2d, e, f) (Additional file 2).
Effects of ADSC-CM collected under different mechanical forces on rat aortic endothelial cells and fibroblasts. a Migration of rat aortic endothelial cells at 12 and 24 h in the scratch wound assay. Scale bar, 200 μm. b Quantitative analysis of the scratch wound assay. cCell proliferation ability of rat aortic endothelial cells at 24, 48 h in the CCK8 viability assay.d Tube formation ability of rat aortic endothelial cells at 6 h in the tube formation assay. Scale bar, 200 μm. e f Quantitative analysis of the tube formation assay. g qPCR analysis of Col I and Col III secretion by fibroblasts. Each experiment was independently repeated three times. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001
ADSC-CM collected under mechanical force promotes collagen secretion by rat fibroblasts
To study the effect of ADSC-CM on collagen secretion, we observed the effect of ADSC-CM collected under different stretching forces on rat fibroblasts. Fibroblasts in the 10% stretch group secreted more Col I and Col III (3.19 ± 0.64, n = 3, p < 0.0001; 4.79 ± 0.21, n = 3, p < 0.0001) (Fig. 2g).
ADSC-CM collected under mechanical force improves skin expansion
Based on the results of the in vitro experiments, ADSC-CM collected under 0% and 10% stretching force was applied to the expanded area in rats. Gross observation of the expanded tissue is shown in Fig. 3a. In each group, images of the expanded skin at different time points were superimposed and the expansion rate on day 30 was calculated (58.65 ± 1.44, n = 3, p < 0.001) (Fig. 3b, c) (Additional file 3). The expansion rate was significantly higher in the 10% stretch group than in the other groups, but did not significantly differ between the 0% stretch and control groups.
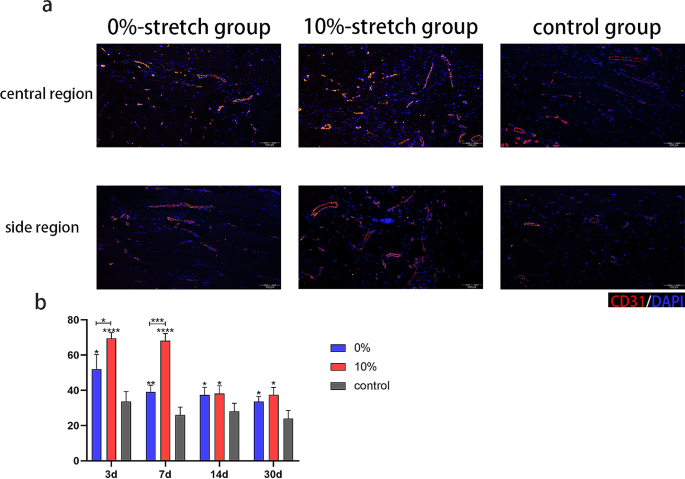
ADSC-CM collected under mechanical force improves vascularization of expanded skin
We performed immunofluorescence staining for CD31 to determine the blood vessel density of central regions. The number of blood vessels was significantly higher in the 10% stretch group than in the other groups at 3 and 7 days, but did not significantly differ among the groups at 14 days (69.50 ± 3.27, n = 3, p < 0.0001; 68.17 ± 4.12, n = 3, p < 0.0001; 38.17 ± 4.49, n = 3, p < 0.05; 37.50 ± 4.18, n = 3, p < 0.05) (Fig. 4).
Assessment of vascularization in skin after expansion in the presence of ADSC-CM collected under mechanical force. a Evaluation of angiogenesis by immunofluorescence staining for CD31 after 7 days of expansion in the central and side regions respectively. Scale bar, 100 μm. b Quantitative analysis of the capillary density of central regions. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001
ADSC-CM collected under mechanical force increases expression of angiogenesis-associated proteins
To elucidate the mechanism by which ADSC-CM collected under 10% stretching force improves vascularization of expanded skin, we investigated expression of selected proteins in expanded skin by qPCR. Expression of VEGF, HGF, and bFGF was significantly higher in the 10% stretch group than in the other groups. (8.16 ± 1.40, n = 3, p < 0.0001; 3.28 ± 0.03, n = 3, p < 0.0001; 2.34 ± 0.20, n = 3, p < 0.01; 1.55 ± 0.22, n = 3, p > 0.05) (Fig. 5).
ADSC-CM collected under mechanical force increases collagen deposition in expanded skin
To evaluate the amount of collagen in expanded skin, immunohistochemical and histological analyses were performed at each time point. On day 30, the levels of Col I and Col III were increased in the 10% stretch group, but did not significantly differ between the 0% stretch and control groups. (44.54 ± 0.51, n = 3, p < 0.0001; 33.33 ± 2.06, n = 3, p < 0.0001) (Fig. 6) Skin thickness did not significantly differ among the three groups. (2.18 ± 0.39, n = 3, p > 0.05) (Additional file 4).
Assessment of collagen deposition in skin after expansion in the presence of ADSC-CM collected under mechanical force. a Immunohistochemistry of Col I after 30 days of expansion. Scale bar, 100 μm. b Immunohistochemistry of Col III after 30 days of expansion. Scale bar, 100 μm. c Quantitative analysis of the levels of Col I and Col III. *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001
Discussion
In this study, we confirmed that mechanical force can regulate the paracrine functions of ADSCs, determined the best mechanical condition to optimize the secretome of ADSCs in order to promote angiogenesis and collagen deposition, and applied ADSC-CM to an expanded area in order to promote skin regeneration (Fig. 7). Our results strongly advocate the application of ADSC-CM collected following mechanical pretreatment for skin expansion because it increases angiogenesis and the collagen content in newly formed skin, does not cause excessive thickening of skin flaps, and thus provides better conditions for expansion of ultra-thin large skin flaps to repair massive soft tissue defects.
Tissue expansion plays an important role in reconstruction of massive skin defects [26]. Application of a tissue expander to exert mechanical force regulates the behavior and function of cells, and thereby promotes tissue regeneration [27]. However, the expansion process takes a long time when simple mechanical stretching is used to stimulate cell proliferation and tissue regeneration. In addition, excessive pressure may cause tissue necrosis due to insufficient blood supply. Therefore, some studies have used MSCs [28] or acellular agents, such as cell-free fat extract, [29] to assist tissue regeneration. However, immune rejection of stem cells and quality control of cell-free liquids hinder their clinical application. Several studies have confirmed that mechanical stimulation is a simple and effective intervention that can control the functions of cells according to its magnitude [14, 30, 31]. Previous studies showed that the paracrine functions of ADSCs can be regulated by changing the mechanical environment to promote wound repair [32]. In the current study, we demonstrated that the paracrine functions of ADSCs can be regulated by adjusting the degree of mechanical force, the secretome can be altered to achieve the desired therapeutic effect, and a higher skin expansion rate can be achieved using ADSC-CM collected under the most suitable mechanical force. To explore the reasons for the increase in the skin expansion rate, we focused on the level of vascularization, which plays an indispensable role in skin regeneration.
Angiogenesis is key to tissue expansion. Tissue necrosis usually occurs when the speed of neovascularization is insufficient for tissue expansion [33]. Therefore, a strategy is needed to promote angiogenesis for tissue expansion. Conditioned medium of MSCs exposed to a suitable level of mechanical force has better angiogenic activity. Nasser et al. demonstrated that secretion of VEGF depends on the stiffness of the matrix and is maximal when MSCs are seeded on hydrogel matrices with a stiffness of 5.0 kPa [34]. Chen et al. found that activation of the Wnt/β-catenin signaling pathway in MSCs exposed to laminar shear stress increases secretion of proteins related to angiogenesis [35]. Previous studies showed that when a full-thickness skin defect is repaired using a hydrogel containing ADSCs and with a stiffness gradient, expression of VEGF in the wound area, vascularization, and wound healing increase [32]. In the current study, we confirmed that ADSC-CM collected following mechanical pretreatment promoted angiogenesis during tissue expansion, possibly due to increased expression of the angiogenesis-related proteins VEGF, bFGF, and HGF. Tissue regeneration requires a variety of biological processes in addition to angiogenesis; therefore, we also studied changes of extracellular matrix components during expansion.
Collagen is the main component of the extracellular matrix in skin; therefore, its secretion must increase during expansion of large skin flaps. Previous studies revealed that mechanically stimulated ADSCs promote collagen deposition in newly formed skin [32]. In the current study, we demonstrated that ADSC-CM collected following mechanical pretreatment promoted collagen expression in regenerated skin. According to histological analysis, the increase of collagen expression did not significantly increase the thickness of the expanded skin flap, which also satisfies the clinical need for construction of an ultra-thin skin flap. These effects may be due to increased expression of growth factors such as bFGF, which promotes proliferation of fibroblasts and regulates expression of collagen [36]. However, the specific proteins involved and their relationship with the optimal degree of mechanical force must be further confirmed experimentally.
The optimal degree of mechanical force to promote the paracrine functions of ADSCs was determined in this study, and the therapeutic effect of ADSC-CM collected under stretching force was preliminarily confirmed by in vivo experiments. Compared to the method of using a tissue expander alone to promote tissue regeneration, incorporating ADSC-CM enhances blood vessel and collagen production during pre-expansion. This reduces the risk of ischemic necrosis and is more advantageous for pre-expanding super-large skin flaps to repair extensive soft tissue defects and refractory wounds. Currently in clinical practice, we mainly rely on the expansive force of expanders to facilitate skin regeneration and achieve large skin flaps. Based on our research findings, while cell-free therapy cannot completely replace current treatments, its auxiliary application can significantly enhance skin expansion efficacy, decrease necrosis rates, and improve overall treatment outcomes. Meanwhile, in contrast with simple stem cell therapy, application of ADSC-CM obtained following mechanical pretreatment avoids safety problems. ADSC-CM does not require immune compatibility to avoid rejection or strictly controlled sterile conditions for its administration, unlike cell-based treatments. Additionally, it minimizes the potential for tumor formation and embolism development associated with stem cell injections [37]. In addition, the quantifiable nature of mechanical force ensures the uniformity and consistency of product content and treatment outcomes. Finally, the study also inspires us to explore the relationship between the optimal degree of mechanical force and intracapsular pressure in the expander in order to reduce the incidence of complications during skin expansion and guide the clinical application of tissue expanders. In the future, ADSC-CM can be combined with rapidly developing green nanomaterials to achieve new breakthroughs in plastic surgery. For example, the combination of mechanically treated CM with biodegradable nano-scaffolds offers great potential. nano-scaffolds provide a biocompatible framework for supporting cell adhesion, proliferation and differentiation, while ADSC-CM promotes the production of blood vessels and collagen. This combined method is very effective for repairing massive tissue defects and complex wounds, and represents one of the important future directions of ADSC-CM application.
There are also some issues to be resolved in the mechanical pretreatment of ADSCs to promote their paracrine functions and thereby skin expansion. It is unclear which components of ADSC-CM play a key role; therefore, it is necessary to further analyze these components and explore the underlying molecular mechanism. In addition, expression of growth factors differs according to the degree of mechanical force applied, and the effects on other aspects of tissue regeneration must be studied.
Conclusion
In conclusion, application of mechanical force to ADSCs increases angiogenesis and collagen secretion by regulating their paracrine functions and thereby promotes skin regeneration and assists skin expansion. This study provides a new strategy to optimize cell-free therapy in the field of tissue regeneration.
Data availability
The data used to support the findings of this study are included within the article.
Abbreviations
- ADSC-CM:
-
Conditioned Medium of Adipose-Derived Stem Cells
- ADSCs:
-
Adipose-Derived Stem Cells
- MSCs:
-
Mesenchymal Stem Cells
- PBS:
-
Phosphate-Buffered Saline
- DMEM/F12:
-
Dulbecco’s Modified Eagle’s Medium: Nutrient Mixture F-12
- DMEM:
-
Dulbecco’s modified Eagle’s Medium
- FBS:
-
Fetal Bovine Serum
- CO2 :
-
Carbon dioxide
- NC:
-
Normal Control
- H&E:
-
Hematoxylin and Eosin
- DAPI:
-
4,6-Diamidino-2-Phenylindole
- cDNA:
-
Complementary DNA
- PCR:
-
Polymerase Chain Reaction
- qPCR:
-
quantitative Real-Time Polymerase Chain Reaction
- SD:
-
Sprague-Dawley
- VEGF:
-
Vascular Endothelial Growth Factor
- bFGF:
-
basic Fibroblast Growth Factor
- HGF:
-
Hepatocyte Growth Factor
- PDGF:
-
Platelet-Derived Growth Factor
- Col I:
-
Collagen type 1
- Col III:
-
Collagen type 3
- Wnt:
-
Wingless/Integrated
References
Tong X, Lu J, Zhang W, Wang S, Huang R, Zhang X, et al. Efficacy and safety of external tissue expansion technique in the treatment of soft tissue defects: a systematic review and meta-analysis of outcomes and complication rates. Burns Trauma. 2022;10:tkac045.
Wang HD, Ibrahim Z, Quan A, Bai J, Ostrander BT, Redett RJ. Pediatric tissue expansion: predictors of premature expander removal in a single surgeon’s experience with 472 expanders. Plast Reconstr Surg. 2020;145(3):755–62.
Handschel J, Schultz S, Depprich RA, Smeets R, Sproll C, Ommerborn MA, et al. Tissue expanders for soft tissue reconstruction in the head and neck area–requirements and limitations. Clin Oral Investig. 2013;17(2):573–8.
Naoum GE, Salama L, Niemierko A, Vieira BL, Belkacemi Y, Colwell AS, et al. Single Stage Direct-to-Implant breast Reconstruction has lower complication Rates Than tissue expander and Implant and comparable rates to Autologous Reconstruction in patients receiving Postmastectomy Radiation. Int J Radiat Oncol Biol Phys. 2020;106(3):514–24.
Lukomska B, Stanaszek L, Zuba-Surma E, Legosz P, Sarzynska S, Drela K. Challenges and controversies in Human mesenchymal stem cell therapy. Stem Cells Int. 2019;2019:9628536.
Turinetto V, Vitale E, Giachino C. Senescence in human mesenchymal stem cells: functional changes and implications in Stem Cell-based therapy. Int J Mol Sci. 2016;17(7).
Han Y, Yang J, Fang J, Zhou Y, Candi E, Wang J, et al. The secretion profile of mesenchymal stem cells and potential applications in treating human diseases. Signal Transduct Target Ther. 2022;7(1):92.
Irons RF, Cahill KW, Rattigan DA, Marcotte JH, Fromer MW, Chang S, et al. Acceleration of diabetic wound healing with adipose-derived stem cells, endothelial-differentiated stem cells, and topical conditioned medium therapy in a swine model. J Vasc Surg. 2018;68(6S):S115–25.
He Y, Xia J, Chen H, Wang L, Deng C, Lu F. Human adipose liquid extract induces angiogenesis and adipogenesis: a novel cell-free therapeutic agent. Stem Cell Res Ther. 2019;10(1):252.
Daneshmandi L, Shah S, Jafari T, Bhattacharjee M, Momah D, Saveh-Shemshaki N, et al. Emergence of the Stem Cell Secretome in Regenerative Engineering. Trends Biotechnol. 2020;38(12):1373–84.
Kandoi LPK, Misra S, Verma RSVKR. The mesenchymal stem cell secretome: a new paradigm towards cell-free therapeutic mode in regenerative medicine. Cytokine Growth Factor Rev. 2019;46:1–9.
Su Y, Xu C, Cheng W, Zhao Y, Sui L, Zhao Y. Pretreated mesenchymal stem cells and their secretome: enhanced immunotherapeutic strategies. Int J Mol Sci. 2023;24(2).
Gorgun C, Ceresa D, Lesage R, Villa F, Reverberi D, Balbi C, et al. Dissecting the effects of preconditioning with inflammatory cytokines and hypoxia on the angiogenic potential of mesenchymal stromal cell (MSC)-derived soluble proteins and extracellular vesicles (EVs). Biomaterials. 2021;269:120633.
Vining KH, Mooney DJ. Mechanical forces direct stem cell behaviour in development and regeneration. Nat Rev Mol Cell Biol. 2017;18(12):728–42.
Yang H, Cheam NMJ, Cao H, Lee MKH, Sze SK, Tan NS, et al. Materials stiffness-dependent redox metabolic reprogramming of mesenchymal stem cells for Secretome-based therapeutic angiogenesis. Adv Healthc Mater. 2019;8(20):e1900929.
Ogle ME, Doron G, Levy MJ, Temenoff JS. Hydrogel Culture Surface Stiffness modulates mesenchymal stromal cell secretome and alters senescence. Tissue Eng Part A. 2020;26(23–24):1259–71.
Li Y, Wu M, Zhang Z, Xia J, Wang Z, Chen X, et al. Application of External Force regulates the Migration and differentiation of adipose-derived Stem/Progenitor cells by altering tissue stiffness. Tissue Eng Part A. 2019;25(23–24):1614–22.
Khalilov R, Bakishzade A, Nasibova A. Future prospects of biomaterials in nanomedicine. Adv Biol Earth Sci. 2024;9:5–10.
Rosic G, Selakovic D, Omarova S. CANCER SIGNALING, CELL/GENE THERAPY, DIAGNOSIS AND ROLE OF NANOBIOMATERIALS. Adv Biol Earth Sci. 2024;9.
Luo Y, Yi X, Liang T, Jiang S, He R, Hu Y, et al. Autograft microskin combined with adipose-derived stem cell enhances wound healing in a full-thickness skin defect mouse model. Stem Cell Res Ther. 2019;10(1):279.
Sha Y, Zhang B, Chen L, Hong H, Chi Q. Mechano Growth factor accelerates ACL repair and improves cell mobility of mechanically injured human ACL fibroblasts by targeting Rac1-PAK1/2 and RhoA-ROCK1 pathways. Int J Mol Sci. 2022;23(8).
Lin LQ, Zeng HK, Luo YL, Chen DF, Ma XQ, Chen HJ, et al. Mechanical stretch promotes apoptosis and impedes ciliogenesis of primary human airway basal stem cells. Respir Res. 2023;24(1):237.
Shan S, Fang B, Zhang Y, Wang C, Zhou J, Niu C, et al. Mechanical stretch promotes tumoricidal M1 polarization via the FAK/NF-κB signaling pathway. FASEB J off Publ Fed Am Soc Exp Biol. 2019;33(12):13254–66.
Liu J, Li Q, Liu S, Gao J, Qin W, Song Y, et al. Periodontal Ligament Stem cells in the Periodontitis Microenvironment are sensitive to static mechanical strain. Stem Cells Int. 2017;2017:1380851.
Ma H, Wang L, Sun H, Yu Q, Yang T, Wang Y, et al. MIR-107/HMGB1/FGF-2 axis responds to excessive mechanical stretch to promote rapid repair of vascular endothelial cells. Arch Biochem Biophys. 2023;744:109686.
Xiong Z, Chen Y, Xu P, Chen C, Xie Y, Chang Y, et al. Regional-controlled tissue expanders increase skin expansion and thickness compared to standard tissue expanders in a rat model. Plast Reconstr Surg. 2022;150(6):1273–84.
He Y, Li J, Liang Z, Tang H, Shi J, Cai J, et al. Internal expansion preconditioning of recipient site increases Fat Graft Retention by enriching stem Cell Pool and Inducing Browning in rats. Plast Reconstr Surg; 2023.
Zhou SB, Chiang CA, Liu K, Li QF. Intravenous transplantation of bone marrow mesenchymal stem cells could effectively promote vascularization and skin regeneration in mechanically stretched skin. Br J Dermatol. 2015;172(5):1278–85.
Deng M, Wang X, Yu Z, Cai Y, Liu W, Zhou G, et al. Cell-free fat extract promotes tissue regeneration in a tissue expansion model. Stem Cell Res Ther. 2020;11(1):50.
Liang X, Huang X, Zhou Y, Jin R, Li Q. Mechanical stretching promotes skin tissue regeneration via enhancing mesenchymal stem cell homing and transdifferentiation. Stem Cells Transl Med. 2016;5(7):960–9.
Driskill JH, Pan D. Control of stem cell renewal and fate by YAP and TAZ. Nat Rev Mol Cell Biol. 2023;24(12):895–911.
Ma Y, Wang Y, Chen D, Su T, Chang Q, Huang W, et al. 3D bioprinting of a gradient stiffened gelatin-alginate hydrogel with adipose-derived stem cells for full-thickness skin regeneration. J Mater Chem B. 2023;11(13):2989–3000.
Wang Q, Zhou L, Wang T, Guo X, Yu H, Wang J. Assisting Rapid Soft-tissue expansion with adipose-derived stem cells: an experimental study in a Pig Model. Plast Reconstr Surg. 2018;142(5):e674–84.
Xue Z, Liao Y, Li Y. Effects of microenvironment and biological behavior on the paracrine function of stem cells. Genes Dis. 2024;11(1):135–47.
Chen W-T, Hsu W-T, Yen M-H, Changou CA, Han C-L, Chen Y-J et al. Alteration of mesenchymal stem cells polarity by laminar shear stimulation promoting β-catenin nuclear localization. Biomaterials. 2019;190–1.
Yang Y, Xia T, Zhi W, Wei L, Weng J, Zhang C, et al. Promotion of skin regeneration in diabetic rats by electrospun core-sheath fibers loaded with basic fibroblast growth factor. Biomaterials. 2011;32(18):4243–54.
Fuentes P, Torres MJ, Arancibia R, Aulestia F, Vergara M, Carrión F, et al. Dynamic culture of mesenchymal Stromal/Stem cell spheroids and secretion of paracrine factors. Front Bioeng Biotechnol. 2022;10:916229.
Acknowledgements
Not applicable.
Funding
This study was supported by College Students’ Innovative Entrepreneurial Training Plan Program (202312121015, S202312121094, 202312121227, 202312121313, 202312121314, 202312121317, 202312121321), National Nature Science Foundation of China (82202474, 82360615), Clinical Program of Nanfang Hospital, Southern Medical University (2022CR007), First People’s Hospital of Yunnan Province (KHYJ-2023-5-02, 2023-KHRCBZ-B14), Guangdong Basic and Applied Basic Research Foundation (2021A1515110440) and Science and Technology Projects in Guangzhou (2024A04J5192, 2023A04J2350, 2023A04J2349, 2023A04J2347, 2023A04J2271).
Author information
Authors and Affiliations
Contributions
ZX carried out the experiments, data analyses and manuscript writing. DH, YZ, participated in the in vitro experiments. MX, HT, participated in the in vivo experiments. YL and YL designed the study and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The project entitled “Mechanical force regulates the paracrine functions of ADSCs to assist skin expansion in rats” was approved by the he Nanfang Hospital Animal Ethics Committee (Approval Number: NFYY20230425034; Date of approval: 2023-07-19).
Consent for publication
All authors agreed to the publication of this paper.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xue, Z., Hu, D., Tang, H. et al. Mechanical force regulates the paracrine functions of ADSCs to assist skin expansion in rats. Stem Cell Res Ther 15, 250 (2024). https://doi.org/10.1186/s13287-024-03822-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-024-03822-0